
PFCC Advisors take inspiring paths coping with grief, loss
Most of us have our own experiences with grieving. What we don’t and will never have is someone else’s experience with grief and loss. Even so, we can often learn from each other’s coping mechanisms, finding a way to apply a version of them in our own lives.
Two members of the Patient and Family Advisory Board at the Comprehensive Cancer Center, Kristin Meekhof and Michele Mitchell, and PFCC Advisor Nancy Maxwell James, found different yet individually fulfilling ways to continue on.
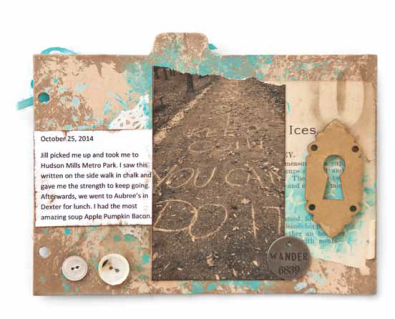
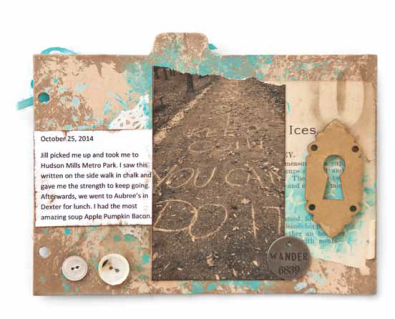
Nancy became part of the PFCC family after suffering a devastating stroke in 2014 and losing the use of her right arm. An artist, Nancy began working in mixed media in 2006, using pieces of antique lace, old photos, buttons and other items in her artwork. She started Sugar Lump Studios while grieving the loss of her dad; “Sugar Lump” was a nickname her mom gave her. Soon, her work was being published.
After the stroke, Nancy longed to get back to her art work and, though physical therapy at UMHS, was able to slowly recover. Below is the text from one of her pieces titled, “Faith Altered Journal.” This work chronicles her path to recovery and faith. It was published in the winter, 2016 issue of Somerset Studio Gallery Magazine. You can read more about Nancy’s artwork and journey at her blog: sugarlumpstudios.com.

-
Kristin is pictured at the 2016 United Nation’s Conference on the Status of Women, where her work was featured.
Kristin, who experienced the loss of her husband from advanced adrenal cancer in 2007, says she found that moving forward in a healthy and meaningful manner requires finding a purpose that is as interesting and intense as the wound one has suffered.
One of the ways she accomplished that was to write a book, “A Widow’s Guide to Healing: Gentle Support and Advice for the First 5 Years”. Meekhof says the book about what she and others experienced, and the lessons that resulted, doesn’t fill the void, but “rests alongside it.”
In the course of writing the book, Meekhof, who holds a master’s degree in social work from the University of Michigan, interviewed more than 100 widows. She also spoke with Dr. Gary Hammer, the director of the Endocrine Oncology Program at the UMCCC.
Next year will mark a decade since the loss of her husband, yet Meekhof says she continues to learn, both from her own experiences and those of others. “I traveled to Kenya and learned from widows about how they live on less than a dollar a day. At the United Nations I learned about 17 sustainable developmental goals, including health and well-being,that can transform the world,” she said.
An in-demand speaker on the topic of grief/loss, she also writes about ways individuals can help in the achievement of these goals. You can visit Kristin’s website and blog here: www.kristinmeekhof.com.

- (l-r) Jennifer Coryell, Tricia Kachin, and Michele Mitchell
Michele and her family found a different way to travel through the grieving process as well as honoring the memory of her stepdaughter, Tricia Kachin. In 2010, at just 20 years of age, Tricia was diagnosed with Stage 4 Hodgkin’s Lymphoma, ironically, from x-rays taken following a car accident. She had been treated for asthma for some time and in retrospect, had all the symptoms of Hodgkin’s, but it had never been diagnosed.
This began a three-year journey on which the entire family travelled. It included a variety of difficult and sometimes, experimental treatments—stem cell extraction, chemotherapy and biopsies—in Houston, New York City, St. Louis and then the University of Michigan. During this time, Trish continued to study cosmetology and to plan her wedding. She had planned one more round of chemo before her wedding. However, during the last chemo treatment, she suffered heart failure, had to go on a ventilator and 10 days later, on July 12, 2014, Tricia’s journey ended.
The family was devastated after such a long struggle, but it was Tricia’s sister, Jennifer Coryell, who came to Michele with an idea to honor Tricia and hopefully, help others. In just a few months, the Kachin Strong Foundation was established.

- Jennifer and Michele at the Kachin Strong Wine Event Fundraiser
The first fundraising event was held in the fall of 2013—a wine tasting. Other events have been held and to date, more than $7,000 has been raised. The Foundation was established to honor Tricia’s memory and create awareness about this disease. The family feels that had Tricia received more of her treatment at UMCCC, she would have had a better chance of survival. Michele and Jennifer, also a PFCC Advisor, are exploring ideas with the CCC to use the funding to honor Tricia’s interest in cosmetology by supporting the wig bank for cancer patients, developing a salon and/or in-room salon services and perhaps someday, an endowment for a medical student scholarship.
Michele said that establishing the foundation has helped the family through their grieving process, by giving them purpose and helping Trisha’s memory live on. She encourages others to keep the stories of their loved ones alive. While the grieving process truly never ends, you do learn to create a “new normal.”
Not everyone wants to write a book – but starting a blog or writing in journal or even on scrap paper might be helpful for some. Starting a foundation won’t appeal to everyone, but finding a way to support a charitable effort in honor of a loved one may bring comfort. For others, it may be setting aside a few minutes a day to read a book or take a walk. The only thing that matters is that it be something that’s important to that individual. Whatever path is chosen won’t begin to fill the void, but it may begin the healing and coping process.
ENTRY FROM “FAITH ALTERED JOURNAL”
By Nancy Maxwell James
 On July 24, 2014, my world changed forever. On a lovely summer afternoon, my motor skills and speech began to falter, an ambulance was called, and I was rushed to the University of Michigan Hospital. I was suffering from an Ischemic stroke. The next three weeks were spent living on the acute rehabilitation floor at the hospital.
On July 24, 2014, my world changed forever. On a lovely summer afternoon, my motor skills and speech began to falter, an ambulance was called, and I was rushed to the University of Michigan Hospital. I was suffering from an Ischemic stroke. The next three weeks were spent living on the acute rehabilitation floor at the hospital.
Since the stroke had occurred on the left side of my brain, it took my functions on my right side. My right arm was completely useless that first week, but my team of occupational therapists were able to get me moving. I told them that I did not care if I could walk again — I just wanted my right arm and hand back so I could make art.
I did not know until returning home that I was looking at a minimum two-year recovery. I had no clue that I would be re-learning how to use my right side. When I was discharged from the main hospital, I was sent to an outpatient program at a local hospital. Twice a week, the ladies there worked their magic, teaching my body how to do things again, and relieving the pain that comes with a stroke.
While my right side is still affected greatly, I am so happy to be able to grasp things with my hand, write a few words at a time (without tiring), and even wash my hair. There was a time I could not even do these simple things. I am hopeful that my recovery and strength continue to grow.
Creating this journal took a few months, but it gave me faith again! All I wanted was to have my art back.
I separated a Kraft chipboard book, and applied paint in layers using bubble wrap and pouncing-brush techniques. I added white paper doilies and cookbook ephemera with matte gel medium. I stamped numbers on page tabs. I printed various photos in a sepia tone on double matte photo paper, cut them out, and inked the edges. I computer generated text to a size compatible with the book size. I then cut out the text, and inked edges. I adhered photos and text to the book pages, and added photo tabs. I adhered buttons, word charms, paper flowers, and other embellishments to the pages. I bound the book with binder rings, and tied assorted ribbons to the rings.



















 On July 24, 2014, my world changed forever. On a lovely summer afternoon, my motor skills and speech began to falter, an ambulance was called, and I was rushed to the University of Michigan Hospital. I was suffering from an Ischemic stroke. The next three weeks were spent living on the acute rehabilitation floor at the hospital.
On July 24, 2014, my world changed forever. On a lovely summer afternoon, my motor skills and speech began to falter, an ambulance was called, and I was rushed to the University of Michigan Hospital. I was suffering from an Ischemic stroke. The next three weeks were spent living on the acute rehabilitation floor at the hospital.